- The structural causes of infertility, recurrent pregnancy loss (RPL), and abnormal uterine bleeding (AUB) cannot be determined by manual examination.
- The best imaging techniques for evaluating the endometrial cavity are hysteroscopy and sonohysterography (SHG) - the latter sometimes called "saline infusion sonography", a contrast ultrasound technique that can also be performed with gel.
- The best techniques for imaging the myometrium are ultrasonography and magnetic resonance imaging (MRI).
- Adenocarcinoma of the endometrium can present in women with chronic AUB (AUB-M) making endometrial sampling necessary in appropriately selected women at increased risk for this diagnosis. This risk is NOT limited to women over 45 or even over 40, it is existent in anyone with long term ovulatory disorders or in those with a related genetic history as well.
The main structural anomalies of the uterus include the spectrum of Müllerian anomalies, while the "acquired" abnormalities include polyps, adenomyosis, leiomyomas, and malignancy, the "PALM" group of FIGO's System 2 also known as the "PALM-COEIN" system. Hysteroscopic surgery is particularly appropriate for polyps, most submucous leiomyomas (Types 0, 1 and 2), and for transection of rASRM Class 5 septums (or CONUTA U2 a & b). However, not all leiomyomas are amenable to hysteroscopic resection and transection of septums must be performed only after confirming that indeed it is an ASRM Class 5/CONUTA U2 anomaly. This process requires a diligent, conscientious, and structured approach using a spectrum of imaging techniques.
Video demonstrating performance of sonohysterography (SHG) and the relationship to an endometrial polyp seen hysteroscopically
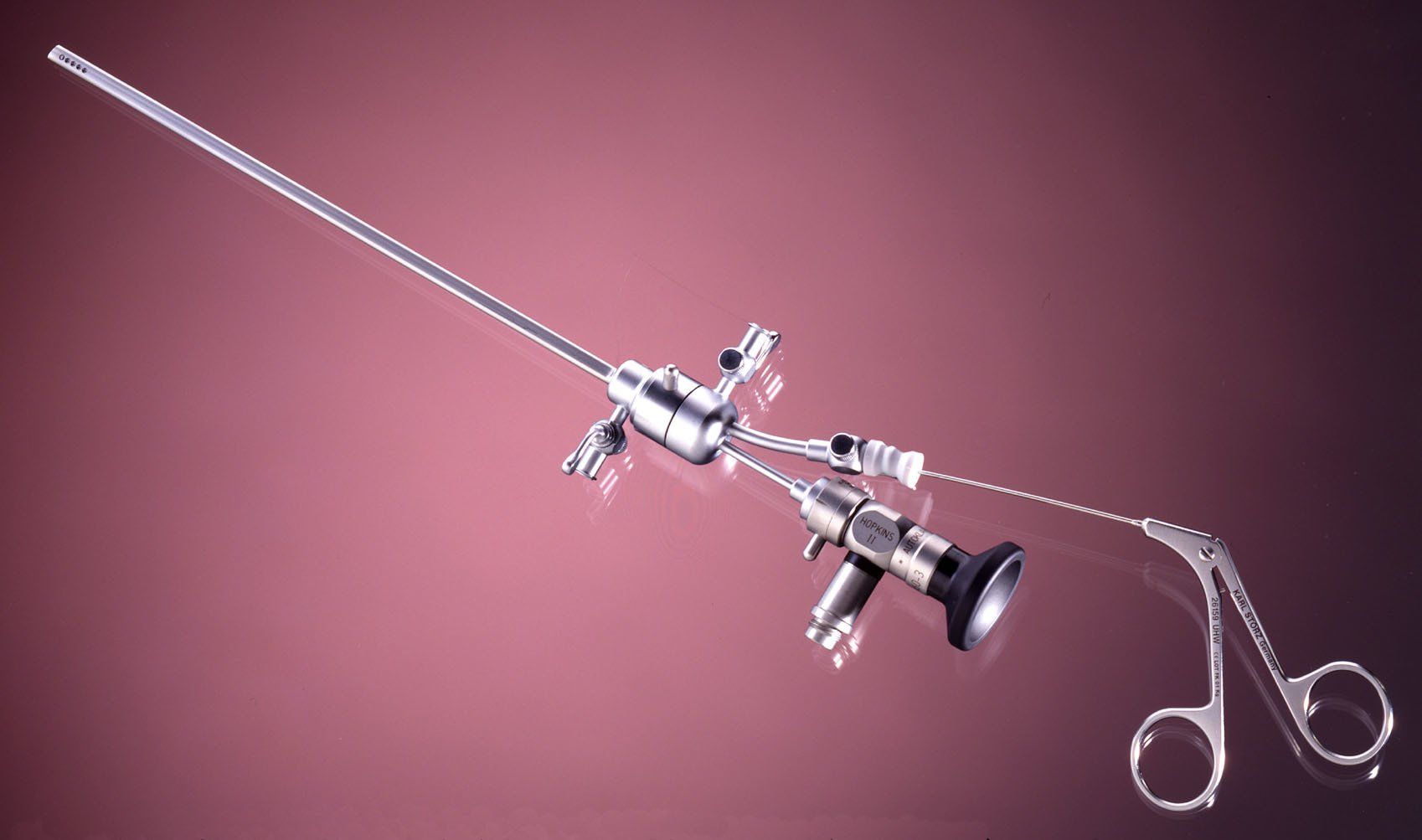
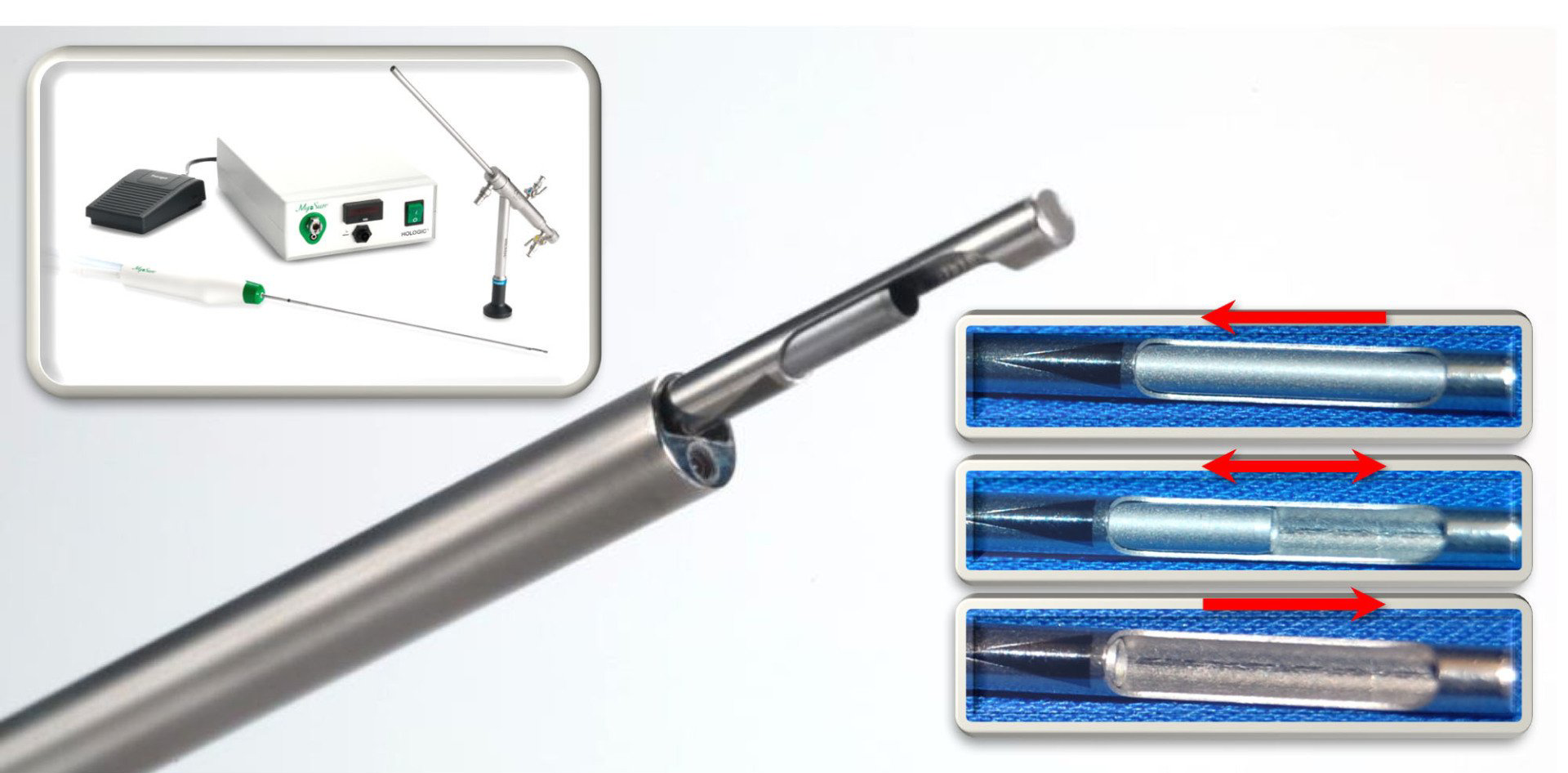
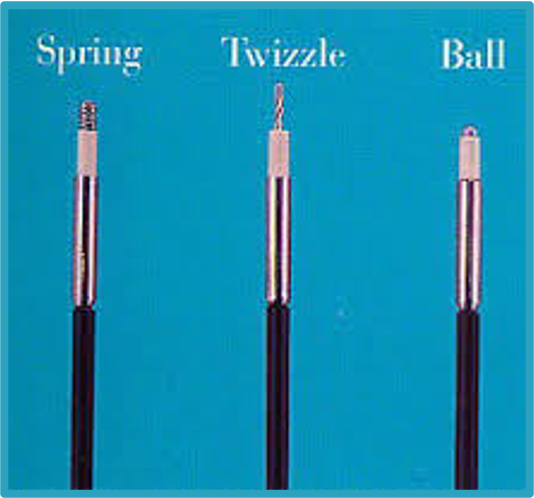
Instruments for Incision, Excision, or Targeted Destruction of Intrauterine Tissue
- Preparation for any surgical procedure, including hysteroscopic surgery, is a strategy that comprises a synthesis of education, communication and a medical process.
- Informed consent is more than a signed document; it is an iterative process that combines questioning, counseling and balancing the risk of an intervention with the anticipated benefit in a way that allows the patient to formulate an informed decision.
- The risks associated with hysteroscopy are real but are minimized if the procedures are performed by individuals with appropriate training who are practicing in an environment with adequate staff, supplies and equipment.
- Regardless, it is important that patients are provided information regarding the risks of hysteroscopic surgery that allow them to make the informed decision.
- There exist a number of medical interventions that may improve the outcome of a hysteroscopic surgical procedure that include suppression of endogenous estrogenic activity to thin the endometrium, ripening of the cervix to reduce the force of dilation and preemptive analgesia to reduce procedure pain if the hysteroscopic intervention is performed under local anesthesia.
- While many women, particularly those who require diagnostic hysteroscopy only, require no analgesia, many require uterine anesthesia be it using local, regional or general anesthetic techniques.
- Anxiety contributes to the perception of pain, so when performing hysteroscopic procedures in an office or clinic environment, efforts should be made to reduce anxiety based on the appearance of the room, its temperature and the general mood which can be affected by noise or other interruptions and the comportment of the medical and support staff.
- Women should be reassured that if the procedure causes undue pain, it will be terminated and plans made to complete it at a later time and possibly under different conditions such as with different anesthesia and possibly in an alternate location.
- There is evidence that music reduces both anxiety and pain.
- There is high quality evidence that, at least for diagnostic hysteroscopy, the vaginoscopic technique is feasible and comfortable for the vast majority of women.
- Local anesthetic techniques, appropriately applied, can allow the performance of the entire spectrum of hysteroscopic surgical procedures. There is increasing evidence that the vagina and the entire uterus should be considered and approach that recognizes the unique and variable innervation of the uterus.
- Regardless of the analgesia or anesthetic technique used women should be encouraged to have a support individual available to accompany them home following the procedure. This is mandatory should psychoactive or systemic anesthetic agents be used for the procedure.
Local anesthesia for intrauterine procedures including hysteroscpoic surgery.
- Without successful access to the endometrial cavity, hysteroscopy is not possible, so careful attention to technique is critical to success.
- There exist a number of techniques whereby uterine access can be achieved and not all are applicable to all patients. Consequently, the effective hysteroscopist should be facile at more than one approach.
- Visual entry using the hysteroscope is the preferred approach; blind entry techniques are to be discouraged
- In some instances access is difficult, a circumstance that may necessitate the use of a number of ancillary techniques including concomitant transabdominal ultrasound.
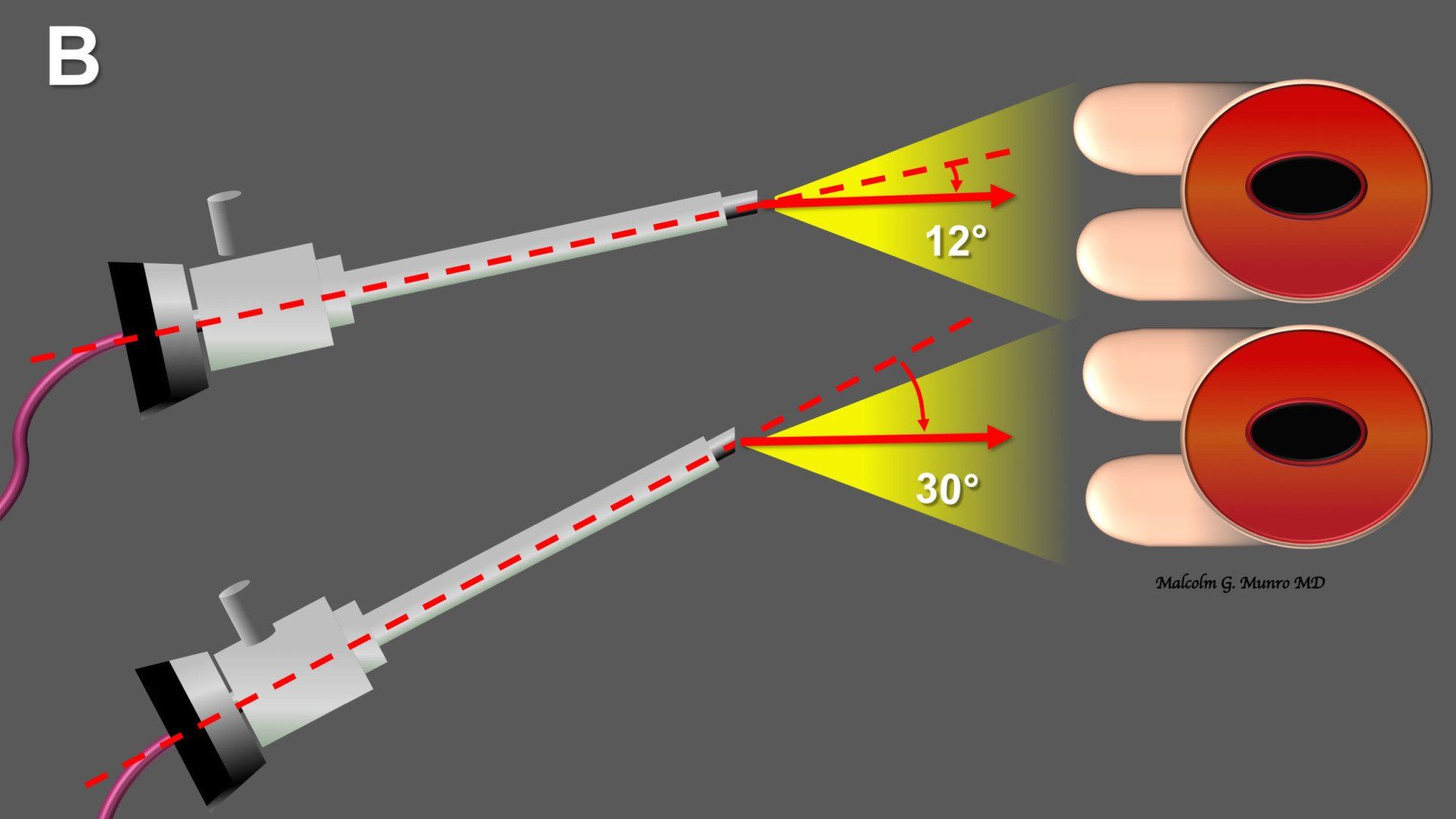
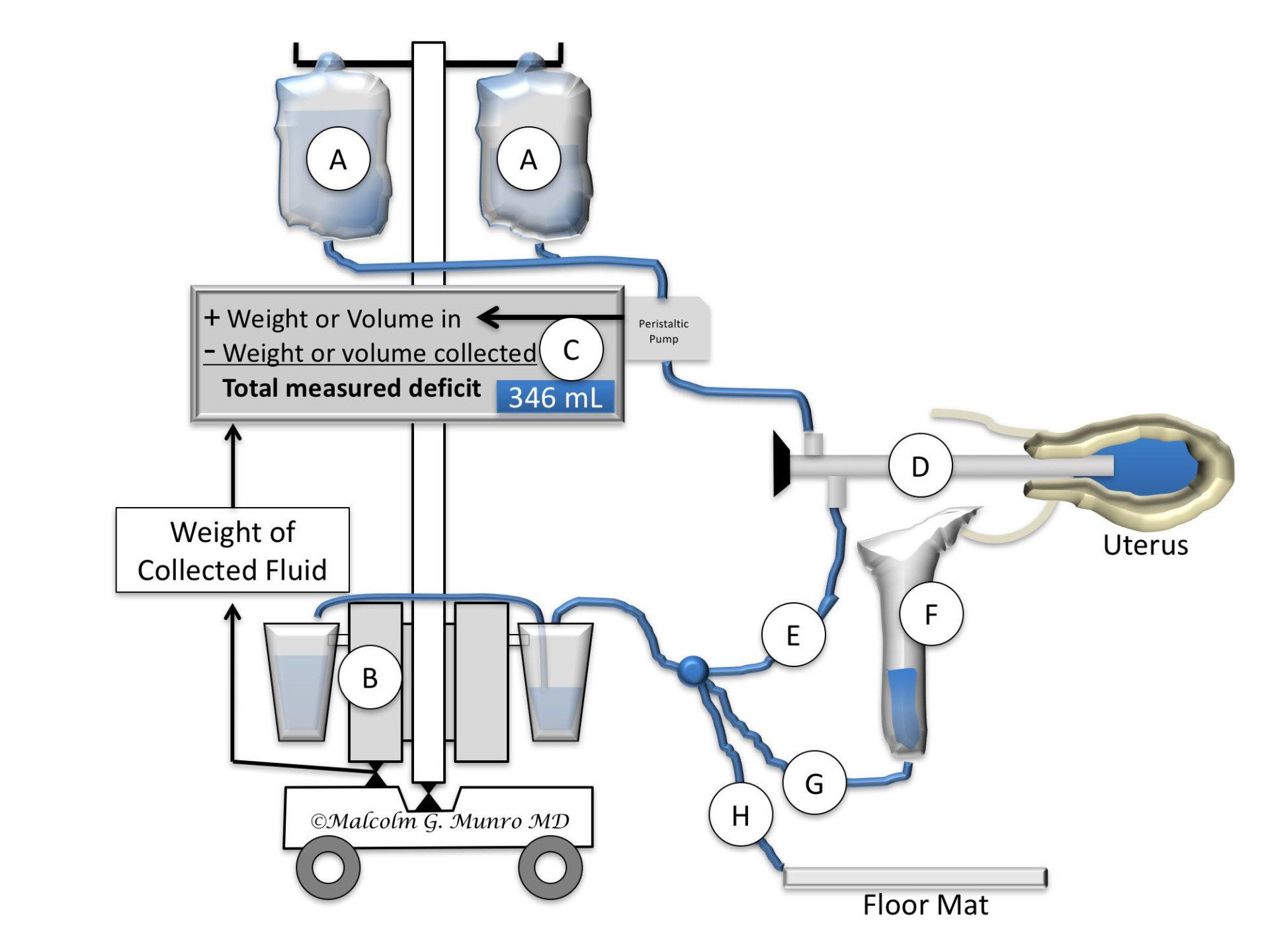
- Distention media are needed for hysteroscopy for the purpose of converting the potential space of the endometrial cavity to a real space
- Options for uterine distention include CO2 and fluid media. CO2 is not suitable for operative procedures
- Hypotonic, non electrolytic fluids solutions containing glycine, sorbitol and mannitol are required for the use of RF electrosurgery with monopolar instrumentation
- Excessive absorption of hypotonic fluids can result in fluid overload and hypotonic hyponatremia, causing permanent neurological complications or death.
- Normal saline is a safer media because, even with moderate levels of absorption, electrolyte levels are normal
- Bipolar RF instrumentation require saline media, a circumstance that makes them safer than monopolar instrumentation when excess media is absorbed into the systemic circulation.
- Distention media management systems that control infusion pressure and monitor systemic absorption are recommended when it is known or suspected that the integrity of the myometrium will be breached during the procedure.
- The maximum allowable absorption of electrolyte free media ranges from 500 mL to a maximum of 1,000 mL
- The maximum allowable absorption of normal saline ranges from 1,500 to 2,500 mL depending in large part on their baseline cardiopulmonary function
- Hysteroscopic programs should have protocols that guide the termination of procedures when the preset thresholds are met
NOTE: All demonstrated procedures have been performed in an office procedure room under local anesthesia
Hystroscopic polypectomy using 5 Fr scissors for transection and grasping forceps for extraction
Hysteroscopic polypectomy using an electromechanical transection and aspiration system.
Intrauterine adhesiolysis with trans abdominal ultrasound guidance
Hysteroscopic transection (NOT resection) of a septum involving the endometrial cavity, without involvement of the cervix.
Removal of products of conception hysteroscopically, rather than blind techniques that appear to increase the risk of post procedure adhesions.
Hysteroscopically directed removal of an IUD from the endometrial cavity
Radiofrequency (RF) loop electrosurgical resection/morcellation of a FIGO Type 1 leiomyoma. Removal of the morcellated fragments, not seen, is performed manually with forceps/curette
Electromechanical removal of a FIGO Type 0 leiomyoma.
SUMMARY and CONCLUSIONS
Hysteroscopic surgery is an essential part of minimally invasive gynecologic surgery (MIGS), being the least invasive of the surgical techniques. There are no visible incisions and the approach allows direct access to pathology that causes symptoms such as AUB, infertility and recurrent pregnancy loss, without the need for transecting the abdomen or the myometrium. Because the access is through pre-existing channels (vagina, cervical canal) hysteroscopic surgery can also be considered a type of "natural orifice" surgery. However, there are perils to hysteroscopic surgery, especially if the surgeon is not careful - both with preoperative evaluation and with surgical techniques. Consequently, it is imperative that women are properly evaluated and surgeons properly trained and experienced in performing these procedures. Indeed, essentially all hysteroscopic procedures can be performed in an office environment without systemic opiates or anxiolytics, an approach that further decreases risk and cost, both to the healthcare system and the patient.